Healthcare employers across the United States face a mounting crisis that extends far beyond traditional staffing challenges. Multi-state licensing and credentialing delays are creating significant bottlenecks in healthcare recruitment, with the average credentialing process taking 90-180 days and costing healthcare organizations an estimated $2.4 million annually in lost revenue and operational inefficiencies.
The complexity of managing healthcare professionals across state lines has intensified as healthcare systems expand their reach, telehealth services proliferate, and the demand for flexible staffing solutions grows. For healthcare employers, understanding and addressing these credentialing challenges isn't just about compliance—it's about ensuring patient access to quality care while maintaining operational efficiency.
What Is the Multi-State Healthcare Credentialing Crisis?
The credentialing crisis stems from a fragmented system where each state maintains independent licensing boards, varying requirements, and different processing timelines. State budgets and lack of staffing are common reasons for delays, with processing speeds varying significantly by state and profession.
This fragmentation creates several critical challenges:
Administrative Complexity: Healthcare organizations must navigate 50 different state licensing systems, each with unique documentation requirements, renewal schedules, and verification processes. License expirations are not uniform across states, with some licenses renewing annually while others operate on biennial or triennial cycles.
Extended Hiring Timelines: The multi-layered verification process significantly extends time-to-hire, leaving healthcare facilities understaffed during critical periods and increasing the burden on existing staff.
Financial Impact: Beyond direct costs, credentialing delays create opportunity costs through unfilled positions, overtime expenses, and potential revenue loss from reduced service capacity.
How Do Multi-State Licensing Requirements Impact Healthcare Staffing?
Quantified Impact on Healthcare Operations
Recent industry data reveals the substantial impact of credentialing delays on healthcare staffing:
- Average credentialing time: 120-180 days for multi-state providers
- Cost per delayed hire: $15,000-$25,000 in lost productivity and overtime coverage
- Revenue impact: Healthcare facilities lose an average of $1.2 million annually per unfilled physician position
- Staff burnout correlation: 73% increase in turnover rates at facilities with prolonged credentialing delays
State-by-State Variation Challenges
The inconsistency across states creates operational nightmares for healthcare employers. While some states process medical licenses within 30 days, others require 120+ days for the same qualifications. This variability makes workforce planning nearly impossible and forces healthcare organizations to maintain larger buffer staff or accept service limitations.
Documentation and Verification Bottlenecks
Managing the vast documentation for multi-state licensing and credentialing is challenging, with missing or incorrect documents leading to rejections and delays. Healthcare employers must coordinate with multiple verification sources, educational institutions, and previous employers across different states, each with varying response times and requirements.
What Are the Root Causes of Healthcare Credentialing Delays?
Systemic Infrastructure Challenges
The healthcare credentialing system operates on outdated infrastructure that wasn't designed for today's mobile workforce. Most state licensing boards still rely on paper-based processes, manual verification methods, and siloed databases that don't communicate with each other.
Resource Constraints at State Level
Many state licensing boards operate with limited budgets and understaffed verification departments. Most states license numerous other professions and occupations, not just those in healthcare, creating competing priorities for limited administrative resources.
Primary Source Verification Requirements
Simply asking healthcare providers to submit diplomas is no longer sufficient for credentialing, as healthcare institutions must check with primary sources regarding education and training. This comprehensive verification requirement, while necessary for patient safety, significantly extends processing timelines.
Lack of Interstate Coordination
The absence of standardized interstate agreements means each state operates independently, requiring healthcare professionals to complete separate applications, pay multiple fees, and undergo redundant verification processes for similar qualifications.
What Solutions Can Healthcare Employers Implement?
1. Proactive Credentialing Strategies
Early Application Submission: Begin credentialing processes 6-9 months before anticipated start dates, accounting for potential delays and resubmission requirements.
Parallel Processing: Submit applications to multiple states simultaneously rather than sequentially, reducing overall timeline despite individual state processing speeds.
Documentation Standardization: Maintain comprehensive, standardized credential files that can be quickly adapted for different state requirements.
2. Technology-Enabled Solutions
Credentialing Management Platforms: Implement specialized software that tracks multiple state requirements, renewal dates, and submission deadlines across all providers.
Digital Verification Systems: Utilize platforms that interface with primary source verification services to reduce manual coordination and human error.
Automated Compliance Monitoring: Deploy systems that provide real-time alerts for expiring licenses, incomplete applications, and state requirement changes.
3. Strategic Staffing Partnerships
Working with experienced healthcare staffing partners can significantly reduce credentialing complexity. Established staffing companies maintain relationships with state boards, understand processing nuances, and can navigate expedited pathways when available.
Benefits of Professional Staffing Support:
- Pre-credentialed provider pools
- Established state board relationships
- Expedited processing knowledge
- Compliance expertise across multiple states
- Risk mitigation for incomplete applications
How Can Healthcare Organizations Optimize Multi-State Operations?
Developing Interstate Compacts Awareness
Several healthcare professions have established interstate compacts that allow providers licensed in one member state to practice in other member states without additional licensing. Healthcare employers should prioritize recruiting from compact-participating states when possible.
Current Healthcare Compacts:
- Nursing Licensure Compact (NLC): 39 participating states
- Physical Therapy Compact: 32 participating states
- Emergency Medical Services Compact: 14 participating states
Creating Credentialing Centers of Excellence
Larger healthcare organizations benefit from centralizing credentialing operations into specialized departments with dedicated staff who understand multi-state requirements and maintain relationships with various licensing boards.
Implementing Risk-Based Credentialing
Adopt tiered credentialing approaches that expedite processing for providers with established track records while maintaining thorough verification for new practitioners.
What Are the Financial Benefits of Streamlined Credentialing?
Return on Investment Analysis
Healthcare organizations that implement comprehensive credentialing optimization strategies typically see:
- 40% reduction in time-to-hire
- $180,000 annual savings per 100-bed facility
- 25% decrease in overtime expenses
- 60% improvement in staff satisfaction scores
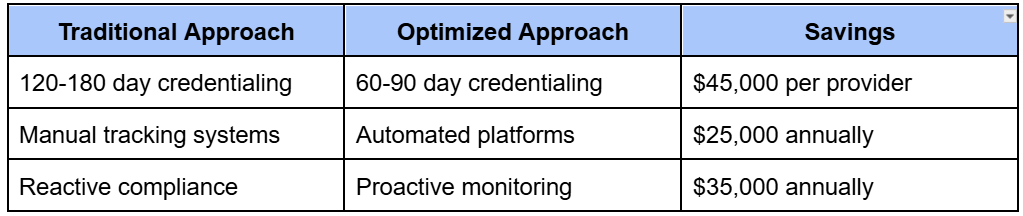
Cost-Benefit Comparison
Frequently Asked Questions
Q: How long should healthcare employers expect the credentialing process to take?
With proper planning and optimization, multi-state credentialing can be reduced from the typical 120-180 days to 60-90 days. However, this requires proactive application submission, complete documentation packages, and experienced navigation of state-specific requirements.
Q: What states have the fastest healthcare licensing processing times?
States with expedited processing include Delaware (15-30 days), Nevada (30-45 days), and Tennessee (30-60 days). However, processing times can vary based on application completeness and seasonal volume.
Q: Can healthcare organizations legally employ providers while credentialing is pending?
Most states allow temporary practice arrangements under supervision while credentialing is pending, but specific requirements vary significantly. Healthcare employers should consult legal counsel and state board regulations before implementing temporary practice agreements.
Q: What documentation causes the most credentialing delays?
The most common delay causes include incomplete malpractice insurance verification, missing educational transcripts, delayed primary source verification responses, and gaps in employment history documentation.
Q: How do interstate compacts affect multi-state credentialing?
Interstate compacts significantly reduce credentialing complexity by allowing providers licensed in one member state to practice in other member states. However, providers must still meet individual state requirements for initial licensing and maintain active licenses in their primary state.
Key Takeaways for Healthcare Employers
The multi-state healthcare credentialing crisis requires proactive, strategic approaches that go beyond traditional compliance thinking. Healthcare employers who recognize credentialing as a strategic operational function—rather than just an administrative necessity—will gain competitive advantages in talent acquisition and retention.
Essential Action Items:
- Implement proactive credentialing timelines (6-9 months advance planning)
- Invest in credentialing management technology and training
- Develop relationships with experienced staffing partners
- Create standardized documentation systems
- Monitor interstate compact developments for expanded opportunities
Strategic Considerations:
- View credentialing optimization as patient care improvement
- Calculate true costs of credentialing delays beyond direct expenses
- Develop contingency staffing strategies for credential-related gaps
- Maintain compliance excellence while pursuing efficiency gains
How DirectShifts Can Help
DirectShifts understands the complex challenges healthcare employers face with multi-state credentialing and offers comprehensive solutions designed to streamline your staffing operations. Our experienced team maintains relationships with state licensing boards across the country and provides pre-credentialed healthcare professionals who can begin contributing to your organization more quickly.
Through our platform, healthcare employers gain access to thoroughly vetted, properly credentialed providers while reducing administrative burden and accelerating time-to-hire. Whether you need temporary coverage during credentialing delays or permanent staff with multi-state capabilities, DirectShifts provides the expertise and support to optimize your healthcare staffing strategy.
Contact DirectShifts today to discover how our credentialing expertise and nationwide provider network can help your organization overcome multi-state licensing challenges and maintain optimal staffing levels.
Discover how DirectShifts can streamline your hiring process and connect you with top-tier clinicians. Experience innovative staffing solutions designed to meet your organization's needs.
Schedule a DemoEmpower Your Healthcare Workforce
Subscribe for industry insights, recruitment trends, and tailored solutions for your organization.













